Etiology
Iatrogenic Causes
- Prolonged catheterization (36%): This treatment causes pressure on the urethra, which causes urothelial necrosis and rubbing or frictional damage to the urethral mucosa from the movement of the catheter.
- Simple Foley catheterization and cystoscopy (12.7%) can cause strictures by harming the urethral epithelium.
- Hypopadias repair: 6.3% of iatrogenic strictures are brought on by hypospadias repair.
- Radical prostatectomy (3.2%): Radical prostatectomy is another cause of urethral strictures.
Inflammatory Causes
Traumatic Causes
The most prevalent cause of posttraumatic anterior urethral strictures is compression of the bulbar urethra against the symphysis pubis, which occurs as a result of straddle injuries. Rarely is this pattern of injury linked to a pelvic fracture.
Pathophysiology
The pathophysiology of urethral stricture involves injury to the urethral epithelium attributed to any of the specific etiologies causing leakage of urine into the corpus spongiosum or by direct trauma to the corpus spongiosum. Either of these etiologies initiates inflammation and fibrous changes in the corpus spongiosum. This fibrous tissue builds up and shrinks, causing contraction and compressing the urethral lumen
History and Physical
Evaluation
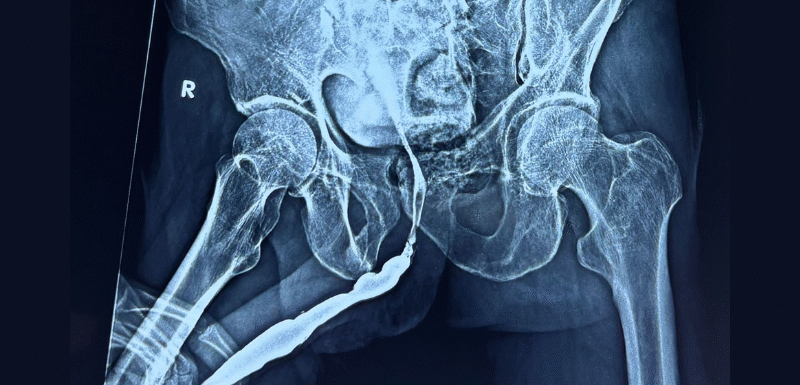
RGU Showing Bulbar Urethral Stricture
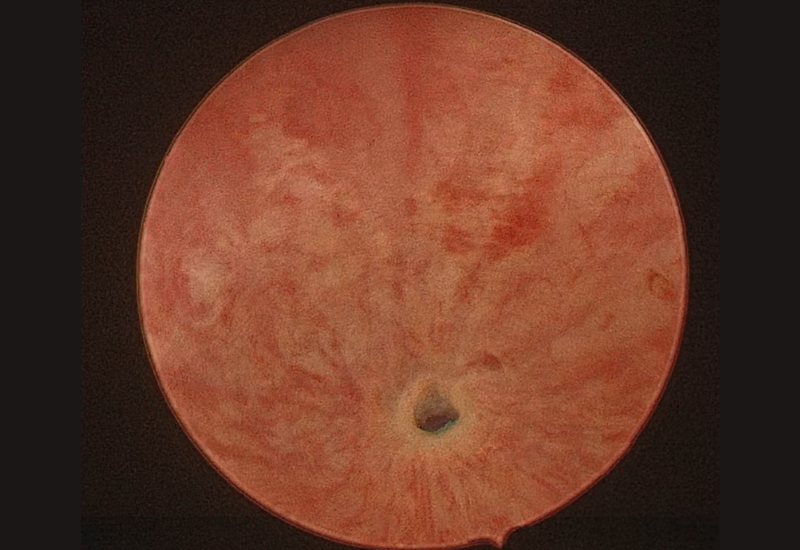
Cystoscopy Image Showing Urethral Stricture
Treatment / Management
VIU
Any penile urethral stricture or bulbar stricture too lengthy for a direct anastomotic urethroplasty should be treated with substitution urethroplasty.
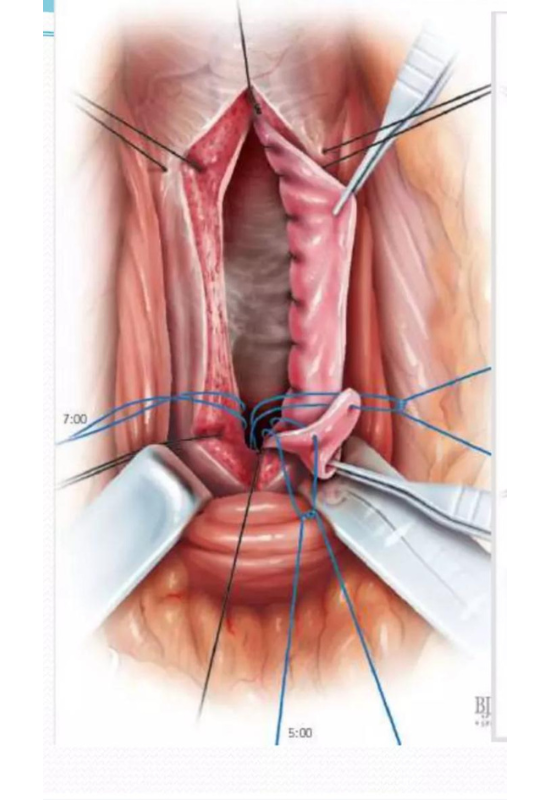 BMG URETHROPLASTY
BMG URETHROPLASTYComplications
- Acute urinary retention
- Bilateral vesicoureteric reflux
- Bladder diverticulum
- Erectile dysfunction
- Penile curvature or shortening
- Recurrent UTIs
- Voiding dysfunction
- Urethrocutaneous fistula