What is Prostatitis?
An infection or inflammation of the prostate known as prostatitis is typically felt in and around the lower pelvic area, usually between the anus and the scrotum. All ages of males are susceptible to it. Men who have discomfort in the muscles and nerves that surround and support the prostate are also referred to by this term.
What are the Symptoms of Prostatitis?
According to the National Institute of Health (NIH), prostatitis exists on a spectrum with pelvic pain
Acute Bacterial Prostatitis (ABP) is an infection of the prostate due to bacteria. Symptoms can come on quickly and include fever, chills, urinary changes, ejaculatory pain and pain in the pelvis or nearby zones, such as the anus. Treatment with antibiotics often leads to quick relief.
Chronic Bacterial Prostatitis (CBP) also occurs from a bacterial infection. Symptoms are often more gradual and may take longer to treat. Fever and chills are not common but pain in the pelvis is still felt along with urinary symptoms and/or ejaculatory pain.
Nonbacterial Prostatitis is inflammation of the prostate that causes pain. It is not due to a bacterial infection and may be from injuries, past urinary tract infections, or prior procedures on the prostate, such as biopsies for cancer.
Chronic prostatitis/chronic pelvic pain syndrome (CP/ CPPS) is a condition that describes discomfort or pain in the area between the scrotum and the anus. It can be from inflammation of the prostate or muscles in that area, which are called the pelvic floor. Nerves that are in the pelvic floor, or go to that area (like from the spine) can also be the cause. Pain from CP/CPPS can last for weeks to months to years. This is NOT an infection but symptoms may be like those in men with CBP.
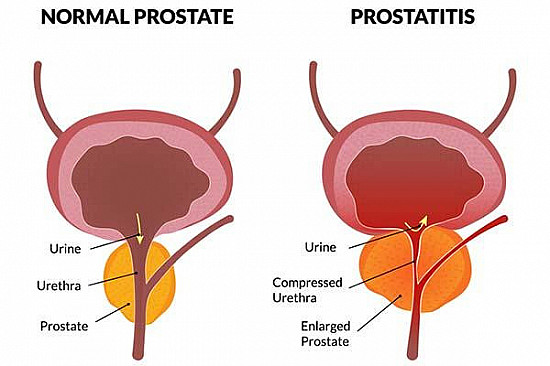
What Causes Prostatitis?
It’s not always clear what causes pelvic pain or prostatitis. A recent operation involving the penis, bladder, or prostate, a bladder infection, a catheter, or a sexually transmitted infection (STI) can all increase the risk of a bacterial infection of the prostate. It may also result from a urinary tract issue unrelated to an infection. However, prostatitis may not be the cause of pelvic pain. Anxiety and stress can also produce symptoms. Additional causes of pelvic discomfort include:
• Pelvic muscle tightness
• Prostate or bladder stones
• Benign prostatic hyperplasia (BPH)
• Urethral stricture (a narrowing or scar of the tube that drains the bladder and runs through the penis)
• Prostate cancer
• Bladder cancer
• Back issues, such a disc herniation or pinched nerve
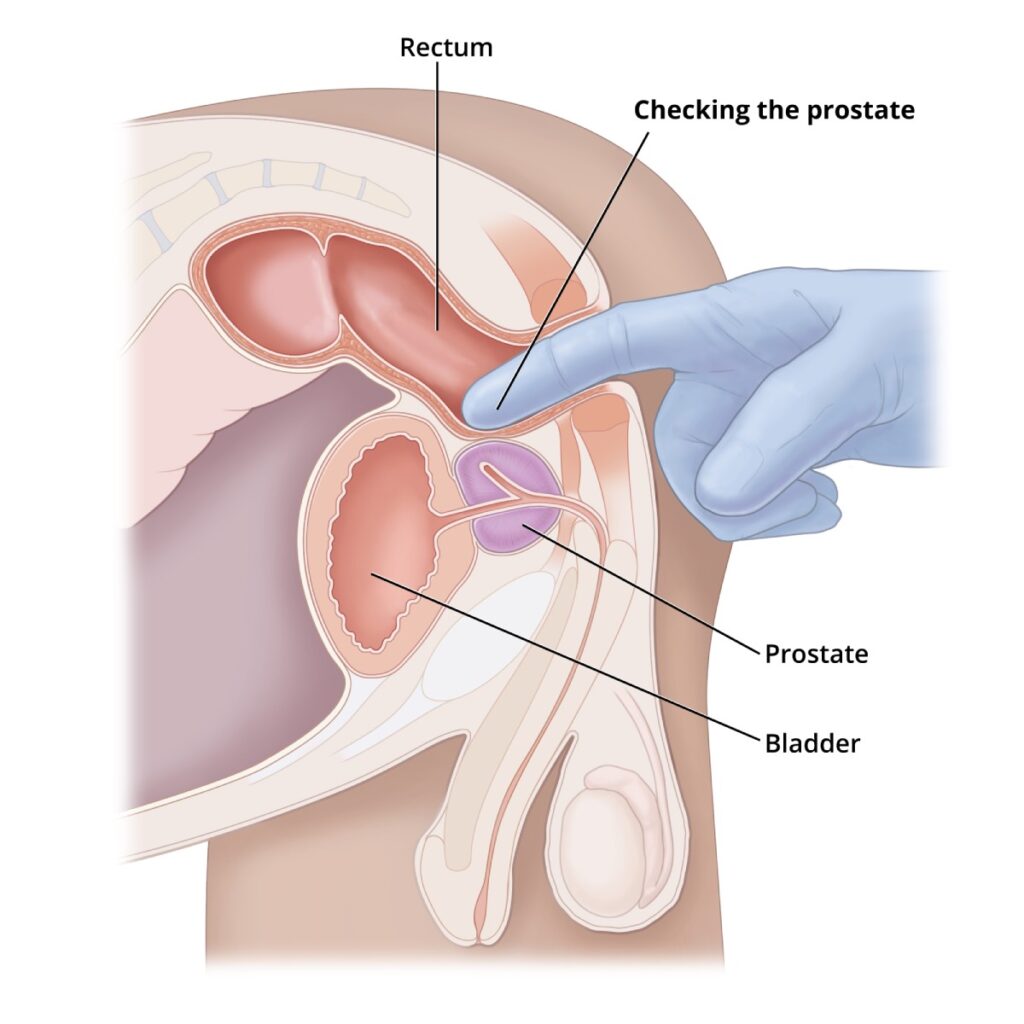
How is Prostatitis Diagnosed?
In order to determine the cause of your discomfort, your healthcare professional may begin by asking you questions. To examine the prostate, a digital rectal exam (DRE) may be performed. Your doctor might perform a cystoscopy to examine your urinary system or a transrectal ultrasound to examine your prostate. In order to monitor your PSA and check for bacteria in your urine or prostate fluid, you can also be required to undergo laboratory testing. To check for a block in your urinary system, a urodynamics test or urine flow study may be performed.
What are My Treatment Options?
Your symptoms, blood results, and visit will all influence how you are treated. Patients may require a variety of treatments. Antibiotics are frequently employed as a first line of defense against any bacteria. Alpha-blockers are medications that may aid in relaxing the muscles at the base of the bladder and surrounding the prostate. Non-steroidal medications known as anti-inflammatory agents are used to lessen muscular or prostate inflammation-related pain. Massage for the prostate: helps reduce prostate pressure. Prostate duct fluid is drained in order to do this. One method to learn how to relax certain pelvic muscles is through pelvic floor physical therapy. It is carried out by a professional to assist you in reducing pelvic floor muscle stress. Trigger point release is one example of this. Home Care: There are numerous methods for easing pain that can be carried out at home. These consist of donut-shaped pillows, heating pads, hot water bottles, and hot baths. Regretfully, tests in medical research have shown no benefit from supplements. Changes in lifestyle, such as nutrition and weight loss, relaxation techniques, pelvic floor exercises, and exercise, can help you feel better and reduce symptoms.
Surgery: on either the urethra or prostate may be needed in rare cases. The medical work up must show a problem that can be fixed. Sometimes, the surgery needed is of the lower back and would be determined by a spine specialist.
Why Choose Us?
Experience and Expertise
Advanced Technology
Personalized Evidence based Treatment
Honesty and Integrity
Affordable Treatments