Prostate cancer
Which tests are used to screen for prostate cancer?
- A blood test called Prostate-Specific Antigen (PSA) measures this protein present in the prostate. Physicians should utilize PSA as the initial screening test for prostate cancer.
- A healthy prostate is indicated by a low PSA score. A large increase in scores could indicate an issue, not always cancer.
- One optional physical examination to check for issues with the prostate is the Digital Rectal Exam (DRE).
- Prostate biopsy:
- If the findings of the PSA and/or DRE testing raise concerns, biopsy tests are used.
- In order to diagnose cancer, a biopsy involves taking a tissue sample from the prostate and examining it under a microscope to look for any cancerous cells.
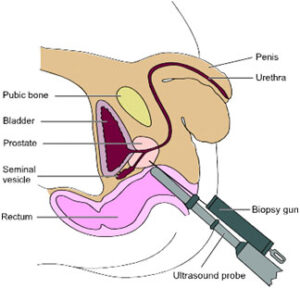
Transrectal Ultrasound Guided Prostate Biopsy
- Imaging and scans may may help your health care team learn more about your cancer. Some types are Magnetic resonance imaging (MRI), Computed tomography (CT) scan and Positron emission tomography (PSMA PET) scan.
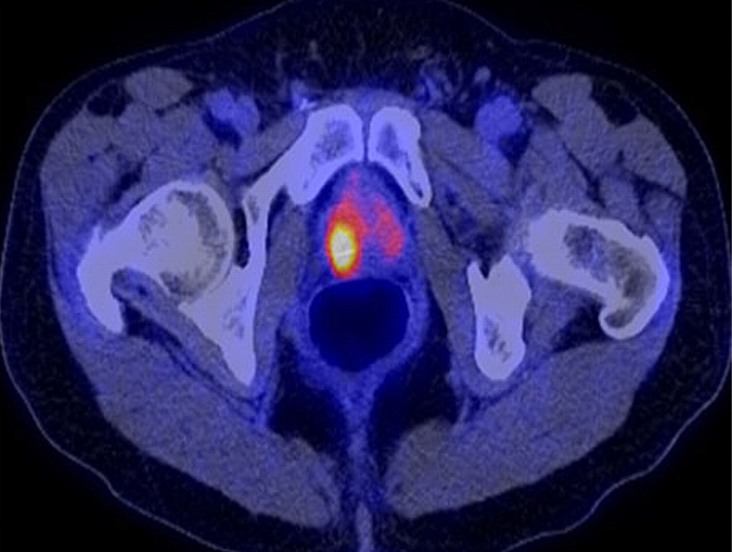
PET SCAN
Risk factors include aging, obesity, family history, high-fat diets, smoking, and inflammation of the prostate. Diagnosis typically involves PSA blood tests, digital rectal exams (DRE), imaging studies, and biopsy. Dr. Vaddi uses advanced tools to detect the cancer’s stage and plan the most appropriate treatment.
What are the Signs and Symptoms of Prostate Cancer?
Why Does Prostate Cancer Occur?
GET TREATED
Active Monitoring
If your cancer is tiny and slow-growing, active surveillance is the best option. Every few months, your doctor will want you to get tests to screen for prostate cancer. A biopsy, an MRI, and a blood test to measure your PSA are typically helpful tests. In most cases, men under active observation can prevent gastrointestinal, sexual, and urine side effects.
Active surveillance
WATCHFUL AWAITING
SURGERY
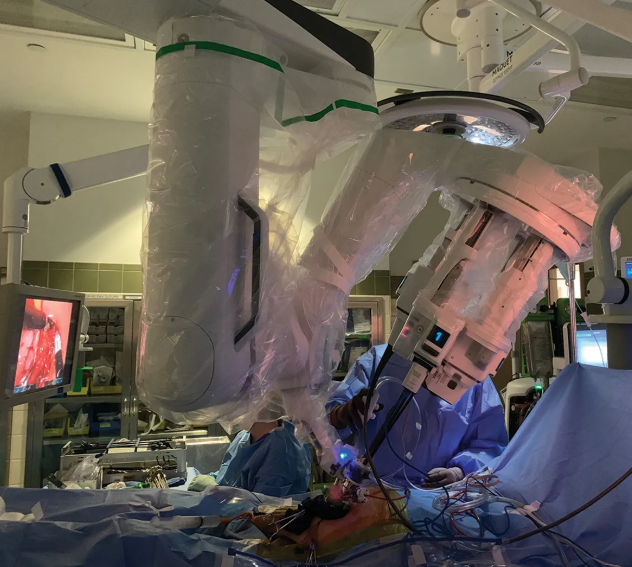
The surgical excision of the prostate, seminal vesicles, and surrounding tissue is known as a radical prostatectomy. The pelvic lymph nodes that flow from the prostate are frequently also removed. Anesthesia and a brief hospital stay are required for this surgery. Four forms of radical prostatectomy surgery exist: • Laparoscopic Radical Prostatectomy with Robotic Assistance (RALP). Five tiny incisions (cuts) are created in the lower abdomen during this procedure, which gives the surgeon access to remove the prostate by guiding equipment and a tiny camera. One of the most popular procedures for treating prostate cancer nowadays is RALP surgery.
Laparoscopic Radical Prostatectomy. This surgery uses a video camera and small surgical tools that fit through cuts in the belly to remove the prostate. This surgery has mostly been replaced with robotic assisted laparoscopic surgery.

Laparoscopic Radical Prostatectomy

Robot Assisted Radical Prostatectomy Specimen
OPEN RADICAL PROSTATECTOMY.
Radical prostrotectamy
Types of Medications
• LHRH/GnRH drugs (androgen deprivation therapy – ADT): LHRH/GnRH are drugs that lower testosterone levels. They may be used whether or not the cancer has spread. There are two types, agonists and antagonists. Agonists (analogs) cause the body to produce a burst of testosterone (called a “flare”). Agonists are longer acting than natural LHRH. After the initial flare, the drug tricks your brain into thinking it does not need to produce LHRH/GnRH because it has enough. As a result, the testicles are not stimulated to produce testosterone. LHRH or GnRH agonists are given as shots or as small pellets placed under the skin. Based on the drug used, they could be given once every one, three or six months. Antagonists also lower testosterone. Instead of flooding the pituitary gland with LHRH, they help limit LHRH from binding to receptors. There is no testosterone flare with an LHRH/GnRH antagonist because the body does not get the signal to produce testosterone. Antagonists may be taken by mouth or injected (shot) under the skin, in the buttocks or abdomen. The shot is given in the health care provider’s office. You will likely stay in the office for a short period of time after the shot to ensure you do not have an allergic reaction. After treatment has started, a blood test makes sure testosterone levels have dropped. You may also have tests to monitor bone density.
• Antiandrogen drugs: Antiandrogen drugs are taken as pills by mouth. These treatments work by inhibiting the androgen receptors in the prostate cancer cells. Normally, testosterone would bind with these receptors to fuel growth of prostate cancer cells. With the receptors inhibited, there is less testosterone to “feed” the prostate. Using certain antiandrogens a few weeks before, or during, LHRH therapy may reduce flareups. Antiandrogens may also be used after surgery or castration when hormone therapy stops working.
• CAB (combined androgen reducing treatment, with antiandrogens): This method blends castration (by surgery or with the drugs described above) and antiandrogen drugs. The treatment reduces
production of testosterone and can help limit it from binding to cancer cells. Surgery or taking oral drugs may be ways to lower the testosterone made by your testicles. The rest of the testosterone is made by the adrenal glands. Antiandrogen therapy limits testosterone made by the adrenal glands.
• Androgen synthesis inhibitors: These drugs help limit other parts of your body (and the cancer itself) from making more testosterone and its metabolites. Those newly diagnosed with metastatic hormone sensitive prostate cancer (mHSPC) or people with metastatic castration-resistant prostate cancer (mCRPC) may be candidates for this therapy.
Hormone Therapy with Surgery
Surgery to remove the testicles for hormone therapy is called orchiectomy or castration. When the testicles are removed, it limits the body from making the hormones that fuel prostate cancer. It is rarely used as a treatment choice in the United States. People who choose this therapy want a onetime surgical treatment. They must be willing to have their testicles permanently removed and must be healthy enough to have surgery. This surgery allows the patient to go home the same day. The surgeon makes a small cut in the scrotum (sac that holds the testicles). The testicles are detached from blood vessels and removed. The vas deferens (tube that carries sperm to the prostate before ejaculation) is detached. Then the sac is sewn up. There are potential benefits to undergoing orchiectomy to treat advanced prostate cancer. It is simple and has few risks. It only needs to be performed once. It is effective right away. Testosterone levels drop dramatically.
Bone-Targeted Therapy
Bone-targeted therapy may help with prostate cancer that has spread to the bones as they may get “skeletalrelated events” (SREs). SREs include fractures, pain and other problems. These drugs may slow the cancer, reduce SREs and help prevent pain and weakness from cancer growing in your bones. Side effects may include flu-like symptoms, bone or joint pain, nausea, diarrhea, and /or feeling weak or tired.