Overview
If you have been diagnosed with Benign Prostatic Hyperplasia (BPH), which is better known as an
enlarged prostate. It is a prevalent aging problem in men. In actuality, BPH affects around half of all males between the ages of 51 and 60. It can affect up to 90% of males over 80.
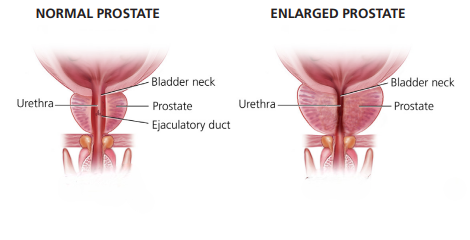
Prostate enlargement is known as BPH. Although an adult man’s prostate is typically the size of a golf ball or walnut, it can enlarge to the size of an orange. The urethra may be squeezed by the gland as it grows. You need to get help right away if you have renal failure or are unable to pass urine at all (a condition known as retention). However, it is frequently possible to watch other symptoms, such as a weak urine stream or the need to push or strain.
Treatment may not be necessary for BPH , but it may be beneficial if symptoms start to appear.
BPH is not harmful. This indicates that it neither causes nor is cancer. However, BPH and cancer can occur simultaneously.
Getting a thorough diagnosis and learning how to relieve your symptoms is really beneficial. We describe the available treatments in this patient guide.
The Prostate: How Does It Function?
The male reproductive system includes the prostate. The primary function of the prostate is to produce fluid for semen. It weighs around one ounce and is around the size of a walnut. It is situated in front of the rectum and beneath the bladder. It passes through a tube known as the urethra. Urine is transported via the urethra from the bladder to the penis.
BPH: What is it?
The expansion of the prostate and surrounding tissue is known as benign prostatic hyperplasia, or BPH. As a man ages, his prostate goes through two major growth phases.
The first occurs when the prostate doubles in size during the early stages of adolescence. The second lasts for the majority of a man’s life and starts at age 25. Your prostate may enlarge with age. When it becomes big enough to cause issues, it’s called BPH.
The urethra is compressed by the growing prostate.
The wall of the bladder thickens. The bladder may weaken and eventually lose its capacity to empty completely. After then, urine stays in the bladder. Many of the lower urinary tract symptoms (LUTS) of BPH are brought on by these issues. Your healthcare team may be able to decide if and what kind of treatment to recommend based on how BPH produces symptoms.
Who Could Develop BPH?
Men over 50, as the risk for BPH increases with age; men whose dads had BPH; men who are obese or overweight; men who don’t exercise regularly; and certain guys who suffer from erectile dysfunction (ED)
What signs of BPH are present?
An enlarged prostate may irritate or obstruct the bladder. Urinating frequently is a common sign of BPH. This could involve having to urinate as frequently as once every two hours, mainly at night.
Below is a list of more BPH symptoms:
• Incomplete emptying: the sensation that, even after urinating, your bladder is full.
• Frequency: the requirement to urinate frequently, roughly every hour to two hours.
• Intermittency: the requirement to repeatedly stop and start the urination process.
• Urgency: the sensation that you must urinate immediately, as if you can’t wait.
• Weak stream: a feeble flow of urine.
• Straining: having difficulty urinating or having to exert effort to do so.
• Nocturia: the urge to get up more than twice during the night in order to urinate
Which factors contribute to BPH?
The reasons behind BPH remain unclear. It mostly affects older men. Changes in hormones are believed to be involved.
Testicular hormones can be the primary cause. For instance, men’s blood levels of active testosterone decrease with age. The amount of estrogen remains constant.
Physical Examination
The next course of action is frequently a digital rectal exam (DRE).
A DRE involves bending over or lying on your side. In order to feel the back wall of the prostate gland, the doctor inserts a gloved, lubricated finger into your rectum. The doctor is searching for lumps, hard areas, discomfort, or enlargement. This 10- to 15-second test is a crucial tool for identifying issues.
Tests of urine
The purpose of these tests is to gauge your ability to discharge urine. This indicates to the physician whether the urethra is obstructed or blocked. There are various kinds:
• A urinalysis examines your urine sample to look for vital components like blood, infection symptoms, glucose (sugar), protein, and other elements that could help your urologist determine the source of your symptoms. Bladder cancer is also detected via urine tests. It’s critical to see your doctor immediately if you have blood in your urine, have pain or burning when passing urine, or are unable to pass urine.
Urine remained in the bladder after passing urine is measured by the post-void residual volume, or PVR. This is done in order to identify the issue. It can also be carried out prior to surgery.
Uroflowmetry is used to quantify the rate at which urine flows. This is done in order to identify the issue. It can also be carried out prior to surgery.
The pressure in the bladder during urine is measured by the urodynamic pressure flow study.
The purpose of these tests is to determine the prostate’s size and form. Among the BPH scans are:
• Ultrasounds, which examine the inside of the body to determine the size and form of the prostate.
• Cystoscopy is an examination that uses a scope to view the bladder or urethra.
• More in-depth scans include computed tomography (CT) and magnetic resonance imaging (MRI). These are carried out in the event that surgery is required to restore urine flow.
An extremely clear picture of the prostate and its surroundings is provided by these scans. It displays the precise location and extent of the prostate’s enlargement.
Blood Examinations
Blood testing might be performed if cancer is suspected.
• Blood tests for prostate-specific antigen (PSA) are used to check for prostate cancer. PSA, a protein produced only by the prostate gland, is measured by the PSA blood test. The lab, hospital, or provider’s office may do this blood test. A few days before the test, refrain from having sex as this could erroneously raise the PSA reading.
Very low PSA is seen in the blood when the prostate is healthy. A rapid increase in PSA could indicate a problem. PSA levels can increase as a result of both benign (non-cancerous) prostate enlargement and prostate inflammation (prostatetitis). Cancer is the most significant factor contributing to an increase in PSA.
GET TREATED
There are many treatments for BPH. You and your health care provider will decide together which option is right for you. Mild cases may need no treatment at all. In some cases, minimally invasive procedures (surgery without anesthesia) are good choices. And sometimes a combination of treatments works best. The main treatments for BPH are:
• Active Surveillance
• Prescription Drugs
• MINIMALLY INVASIVE Surgery :
LASER SURGERY:
HOYAG
THULIUM
KTP/LBO
NON LASER SURGERY:
BIPOLAR TURP
TUMT
TUNA
TUIP
PUL
Prescription medications
For men with BPH, prescription medications may potentially be an option. Among the drug types are:
Alpha blockers are medications that relax the muscles in the bladder and prostate to lessen the symptoms of BPH.
They may increase urine flow in the event of a blockage, but they do not reduce prostate size. Alpha blockers have the advantage of acting immediately. Dizziness, lightheadedness, exhaustion, and trouble ejaculating are possible side effects. Good candidates are men who have moderate to severe BPH and who find their symptoms bothersome. If you are going to have cataract surgery soon, alpha blockers are not a smart option.
Alfuzosin, doxazosin, silodosin, tamsulosin, and terazosin are examples of alpha-blocking medications.
5-Alpha reductase inhibitors are medications that, by inhibiting DHT, can reduce prostate size and increase urine flow. One male hormone that may contribute to prostate enlargement is DHT, which can accumulate in the prostate. These medications may reduce the chance of developing BPH issues and requiring surgery. Erectile dysfunction and decreased libido (sex drive) are among the side effects. To keep the symptoms from returning, you must continue taking the medication. Men with particularly big prostate glands might benefit most from these.
These prescription medications, which include finasteride and dutasteride, may take many months to fully take action.
Both an alpha blocker and a 5-alpha reductase inhibitor are used in combined therapy. They might prevent BPH from worsening more effectively when taken combined than when taken separately.
You can experience more adverse effects from taking two medications than from taking just one. Dizziness, erectile dysfunction, weakness or lack of energy, and a dip in blood pressure while rising up after sitting or lying down are a few possible adverse effects. Antimuscarinics may be prescribed by a urologist to patients who exhibit signs of an overactive bladder. Uncontrollably tight bladder muscles are known as overactive bladder.
Urine is frequently and urgently needed as a result. It may result in leakage, or incontinence. The bladder muscles are relaxed by antimuscarinics.
This treatment works well for guys with bigger prostates.
Finasteride and doxazosin; dutasteride and tamsulosin, a combination of the two drugs that comes in a single tablet; alpha blockers and antimuscarinics are examples of potential drug combos.
prostate urethral lift (PUL):
Tiny implants are inserted into the prostate using a needle during a prostate urethral lift (PUL). The enlarged prostate is lifted and compressed by these implants, removing its obstruction of the urethra. These implants are difficult to remove and remain in the body indefinitely.
Both local and general anesthesia can be used for PUL.
The body is not sliced during this procedure, and no tissue is removed or destroyed. Numerous men with urinary problems and enlarged prostates make excellent candidates. Compared to other forms of prostate surgery, this has fewer sexual adverse effects. If you had a PUL, you may still get an MRI. Discuss with your physician whether you are allergic to nickel, titanium, or stainless steel, as well as how PUL may affect the quality of images from upcoming MRIs required to diagnose prostate cancer. Future research could aid in determining long-term durability, as current studies have assessed PUL therapy for five years.
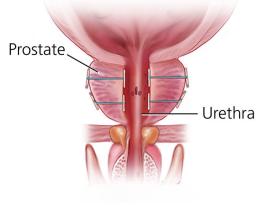
PUL Procedure
Water vapor (steam) is used in water vapor thermal therapy (WVTT) to kill prostate cells that are compressing the urethra.
This procedure can be performed under local anesthetic in a doctor’s office or following a pain medication. It makes use of a unique portable instrument with a needle on the end. It produces steam by combining water and radiofrequency energy.
Rapid cell death is caused by the steam and needle. The prostate shrinks as a result of the dead tissue being broken down and eliminated by the body’s natural healing reaction.
If men have tried prescription medications and found them ineffective, or if they do not want to take medication for BPH, they might be suitable candidates. Men who wish to prevent sexual side effects or who would rather not undergo surgery might also make suitable candidates.
You might need to use a catheter for a few days if you have blood in your pee. Urination that is painful or frequent should stop in two to three weeks. Erectile dysfunction and other sexual adverse effects are unlikely.
According to recent research, symptom relief lasts for a minimum of five years.

REZUM Therapy
TURP:
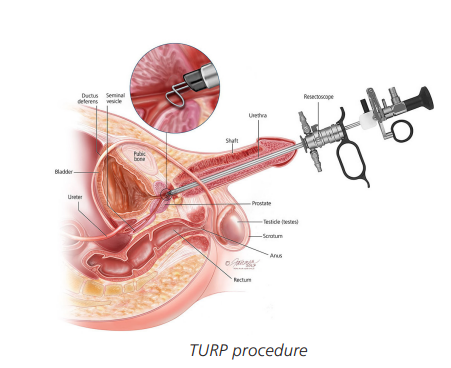
One typical procedure for BPH is transurethral resection of the prostate (TURP). TURP cuts and removes tissue using laser light or electric current. Anesthesia and a device known as a resectoscope that is placed through the penis are used for this. The resectoscope has an electrical loop, light, and irrigating fluid. The loop closes blood arteries and slices tissue. A catheter is used to flush the excised tissue into the bladder and out of the body. TURP may be an excellent option for men who need surgery for moderate to severe BPH symptoms.
The procedure known as “holmium laser enucleation of the prostate” (HoLEP) involves a surgeon inserting a resectoscope into the urethra through the penis. Excess prostate tissue is destroyed using a laser that is placed inside the resectoscope. There is extremely minimal bleeding and no need for incisions or cuts. You might just require a single hospital stay. Although a catheter is utilized, it is often taken out the next day. This treatment might be a suitable option for men with bigger prostates who want to avoid more invasive surgery. HoLEP may also be appropriate for men who are at a higher risk of bleeding, such as those who are on blood thinners.
Simple prostatectomy removes the entire prostate gland with laparoscopic or robotic-assisted surgery. It is important for the surgeon to be skilled at this surgery. This is only offered to men with the largest of prostate glands. This is a long- term cure. You will probably stay in the hospital for a few days after surgery and your activities will be limited for several weeks. A catheter will usually be needed for 1 to 2 weeks while you heal.
Thuflep/holep: The procedure used in HoLEP, ThuLEP, and ThuFLEP surgeries is the same. In other words, aside from the types of lasers utilized in these procedures, known as laser prostatectomy, the surgical approach and methodology are the same. Surgery is carried out under either spinal anesthesia or full anesthesia (general anesthesia) following the anesthesiologist’s evaluation of the patients based on their present illnesses and circumstances. Using camera instruments, the external urinary tract in the penis is entered to begin the procedure. A camera is used to visualize the bladder, the external urinary tract, prostate tissue, and the structure known as the sphincter that permits urine retention. Next, without passing beyond the sphincter, the prostate adenoma is drawn away from the structure known as the capsule using a thulium fiber laser. When we compare this prostate to an orange, the adenoma, or fruit, is removed, leaving behind the capsule, or shell. The orange’s fruit is roughly peeled off, leaving the peel behind. In the meantime, the thulium fiber laser in particular continually releases energy that is absorbed by low-energy water, which lessens bleeding. After exiting the capsule, prostate adenomas are either transported in whole or in small parts to the bladder. Using a device known as a morselator, these portions are reduced in size in order to remove them from the bladder using the force of suction. After being removed, the components are submitted to the lab for pathological analysis. The catheter is then placed into the bladder, and the procedure is over.

Specimen showing thulium fiber laser enucleation of prostate
Why Choose Us?
Experience and Expertise
Advanced Technology
Personalized Evidence based Treatment
Honesty and Integrity
Affordable Treatments