1. Understanding Urinary Incontinence:
Urinary incontinence is the loss of bladder control, leading to accidental urine leakage. It can affect people of all ages and may result from various factors such as aging, childbirth, prostate issues, or neurological conditions. At our hospital, we provide personalized care to help patients regain control and improve their quality of life.
2. Comprehensive Diagnosis:
3. Advanced Treatment Options:
4. Personalized Care and Support:
Why Choose Us?
What is Urinary Incontinence?
- Urinary incontinence is a problem with the loss of control when you pass urine. There are two main types of urinary incontinence:
- Stress urinary incontinence (SUI) is when urine is released, without control, during activity. This happens when the pressure on your bladder increases. An example of this is when you cough, sneeze, or laugh.
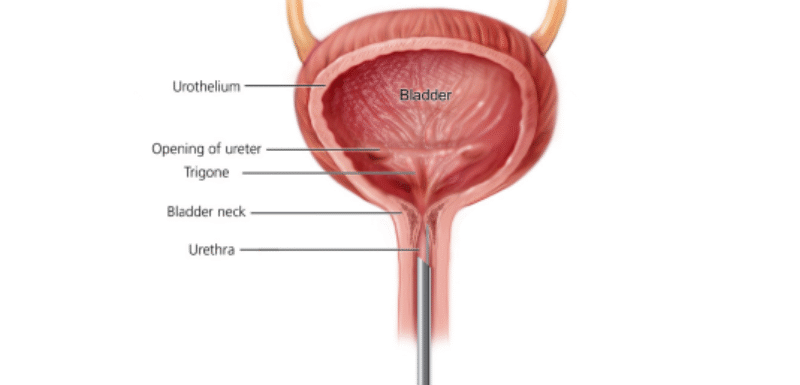
- Overactive bladder (OAB) is a sudden, uncontrollable need to pass urine. The difference between SUI and OAB is anatomical. SUI is a urethral problem. OAB is a bladder problem. SUI happens when the urethra cannot stop the sudden increase in pressure. This can happen when you cough or bend over. With OAB, the bladder will spasm and squeeze uncontrollably and force urine out the urethra. Many people with SUI also have OAB. When they have both types of incontinence, it is called “Mixed Incontinence”.
What is SUI?
Urine leakage caused by abrupt pressure on the bladder and urethra, which causes the sphincter muscle to momentarily open, is known as stress urinary incontinence (SUI). Sudden forceful activity, such as coughing, sneezing, laughing, or exercising, might cause pressure in those with mild SUI. You might also leak when performing less strenuous activities like standing, walking, or bending over if your SUI is moderate or worse. There may be a few droplets or enough of these “accidents” to seep through clothing. SUI affects more people than you may imagine. This issue affects almost one in three women at some point in their life. Although it is less prevalent, men can have SUI. Men may experience issues following surgery or as a result of an injury. If you experience incontinence symptoms, you must be your own best advocate. You can better control your symptoms if you know what to look for and what to anticipate.
SUI Signs and Symptoms
To know if SUI is a problem for you, ask yourself:• Am I afraid to be too far from a bathroom or a change of clothes?• Have I stopped exercising or playing sports?• Have I changed the way I live because I am afraid of urine leakage?• Have I become uncomfortable with my body?• Have my symptoms changed my relationships with friends or family?• Am I avoiding sex because I am worried that I will leak and become embarrassed?
How is SUI Diagnosed?
It is of great value for your health care provider to know if you feel your urine leaks are a
problem. Don’t be embarrassed – providers are trained to talk about these matters! You may be referred to a specialist, such as a urologist or a gynecologist who specializes in incontinence. Some may even have extra certification in Female Pelvic Medicine and Reconstructive Surgery (FPMRS). There are a few things your provider may want to discuss to help make a diagnosis. Your doctor may ask about your urinary symptoms (When do you leak? How often? How much?).Your provider may also review your medical history, perform a physical exam and may ask for tests to find the cause of leaks. For women, your physical exam may include checking your abdomen, the organs in your pelvis and your rectum. For men, it may include checking your abdomen, prostate and rectum. Your provider may also test the strength of your pelvic floor muscles and sphincter muscles. It may also be helpful to keep a bladder diary before you see your provider. A bladder diary is a way to track how much you drink and when. It is also used to track when you have leaks and what may cause them over a period of time. This diary can give your provider clues about what is happening. You and your health care provider may review it together.
Tests
Your provider may order tests to confirm the diagnosis of SUI and rule out other reasons for your urine
leaks.Some tests for SUI are:
• Urinalysis or urine sample which tests for a urinary tract infection or blood in the urine.
• Bladder scan to show how much urine stays in your bladder after you pass urine.
• Cystoscopy uses a narrow tube with a tiny camera to see into the bladder to rule out more serious
urinary tract problems.
• Urodynamic tests tell how well the bladder, sphincters and urethra hold and release urine.These tests can
show how well the bladder works and may help find the cause of leakage.If your provider believes that you
may need surgery to address SUI, these studies may be done.
Surgical Treatments
Slings
Female Sling
The most common surgical treatment for female SUI is the midurethral sling surgery. For
this, a strip of soft permanent mesh is placed under the urethra to support urethral closure during activity (coughing, sneezing, bending, lifting, jumping and running). It is a simple 20-30 minute, outpatient procedure with a small single cut in the vagina. This is easily done under limited anesthesia and linked to a very quick return to normal day-to-day activities. Long-term success rates are in the 90%. Another type of female sling surgery, the
pubovaginal sling, is a bladder neck sling. Here the tissue used to make the sling comes from the patient’s abdominal wall (fascia), or donated tissue (bovine or cadaver).

Mid Urethral Sling
Male Sling
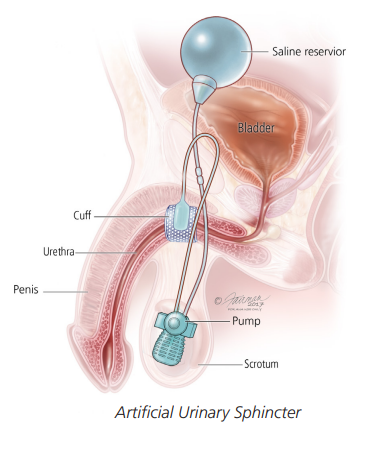
Some men may be offered a sling surgery to treat SUI. The purpose of the male sling is to support the urethral sphincter muscle. This is accomplished by making a cut between the rectum and scrotum and placing a soft mesh tape beneath the urethra. By pushing up on the urethra and generating some coaptation (closing) of the urethra to avoid leaks, it supports the urethra and sphincter muscle. Find out from your doctor if this is something you can do.
Bladder Neck Suspension / Colposuspension
For female SUI, the Burch Colposuspension, also known as bladder neck suspension, is a surgical procedure that uses permanent stitches to raise the neck of the bladder up towards the pubic bone. This is a more extensive procedure that involves cutting through the muscles and skin of the abdominal wall to access the deeper pelvic regions. Compared to the less invasive midurethral sling, this procedure requires more time to heal due to the abdominal incision, but it may be the best option for certain people. It can occasionally be done laparoscopically,
which shortens the recuperation period following surgery.